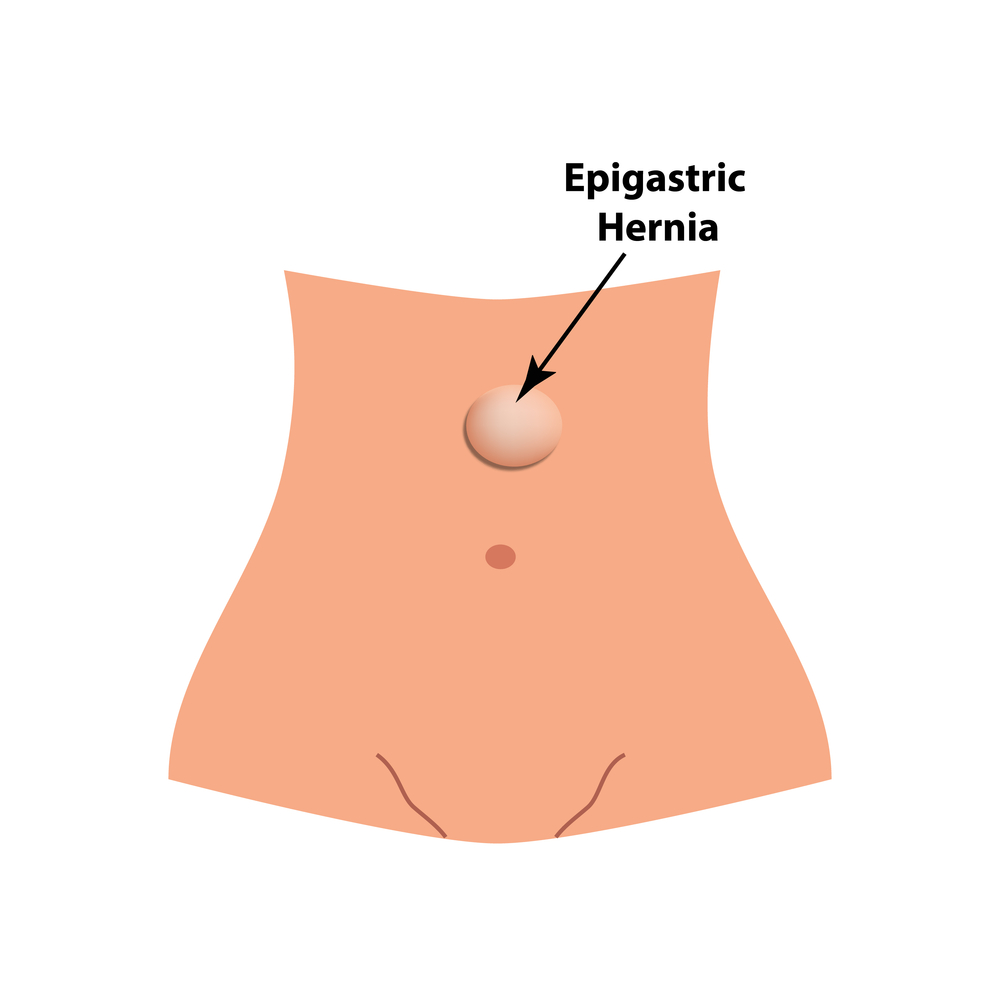
Epigastric hernia repair is typically one of the simplest and safest operations among all hernia procedures. It is an operation that takes less than one hour and can be performed outpatient in a hospital or surgery center. It is usually performed under general anesthesia. It can be performed with conventional open techniques or with the latest robotic technology.
The conventional
open technique is the most common and appropriate technique for typical small epigastric hernias. It involves a small incision over the hernia. The incision is made as small as possible with an emphasis on an optimal cosmetic outcome. The hernia is exposed with delicate and meticulous technique. After complete exposure of the hernia defect and reduction of the hernia contents, the hernia is repaired with a sewing technique without the use of mesh and in some cases mesh is used to help prevent the risk of hernia recurrence. The use of mesh in epigastric hernias remains a topic of great controversy among hernia specialists. After repair of the hernia defect, the subcutaneous tissue and skin is reconstructed with a strong emphasis on optimal cosmetic outcome.
The
robotic repair is a minimally invasive technique appropriate for larger epigastric hernias. This involves general anesthesia and three half inch incisions on the right or left side of the abdomen. An ultra high definition 3d camera is inserted through one of the incisions and different instruments (scissor, clamps, or sewing needle holders) are inserted through the other two incisions. The camera and the instruments are attached to a robotic arm system. The surgeon controls everything while sitting in a console with a 3D viewer and sophisticated hand controls and multiple foot pedals. Ultimately the hernia is well exposed and sewn closed and usually a mesh is sewn below the area to reinforce the repair. The technology allows for unsurpassed vision and delicacy in the repair that yields a less painful result than laparoscopic surgery from the recent past.